Glaucoma Exam in Metro Detroit
What is Glaucoma?
Glaucoma is a category of diseases of the optic nerve (the nerve inside the eye) that slowly causes vision to decline, leading to blindness. i. Known as somewhat of a mystery to eye doctors, glaucoma is a disease of the optic nerve that can lead to blindness. Although it is impossible to pinpoint exactly what causes glaucoma since there are many different forms, we do know that they all cause slow deterioration of the optic nerve. The scary news is that glaucoma can eventually lead to blindness. In fact, glaucoma is the second leading cause of blindness in the world! Glaucoma usually starts by affecting peripheral (side) vision and then continues on to affect central vision. Glaucoma is often associated with a high “intraocular pressure, the pressure inside the eye.
Wait a second! What does it mean to have high pressure inside my eye? Exactly what it sounds like! Imagine holding the center of a hose or faucet that is turned on full blast. Pressure builds up to the point where you find it difficult to continue holding onto the nozzle! If there is a buildup of fluid in the eye, known as aqueous humor, it causes a buildup of pressure. This puts a lot of stress on your optic nerve, causing the damage your doctor will see if you have glaucoma.
Risk Factors for Glaucoma
Unlike with pink eye or an eye injury, glaucoma usually has NO symptoms in its early stages. Although this may sound like a good thing – it’s not! If you don’t notice you have glaucoma early on, the glaucoma can get worse and worse before you notice you even have a problem! Then, by the time you start to see signs, you will have already lost a SIGNIFICANT amount of your vision. Not an easy fact to hear.
The good news is that certain risk factors like age, race and sex will alert your eye doctor to carefully screen you for glaucoma at your annual check-up. Be sure to get your eyes examined annually by an eye doctor.
There is no single test that can be used to diagnose glaucoma. There are, however, several different methods to check if you have developed any early signs of the disease. The first line of defense is checking your eye pressure. A higher eye pressure than normal is the first sign that you may have glaucoma. Another test eye doctors perform regularly is called a “visual field”, a test to check your side vision. As mentioned, side vision is commonly the first to go if you develop glaucoma. Glaucoma is suspected once your doctor sees that you have a certain pattern of decreased side vision.
Glaucoma Treatments
1. There’s good news and bad news. The bad news is that there is no cure for glaucoma. Once the damage is done, it’s irreversible. This is a BIG problem. The good news is that treatments that lower the eye pressure have been shown to slow down the progression of vision loss. The sooner your glaucoma is found, the sooner treatment can begin. So don’t wait!
Oftentimes, if you have certain risk factors for glaucoma, your eye doctor will consider you a glaucoma suspect, and will follow you very carefully. This way, if glaucoma develops, it can be treated right away.
The 3 types of treatments available are 1. Eye drops, 2. Laser treatments or 3. Surgical procedures.
Drops are the most common first line of treatment. They can be dosed anywhere from one to four times per day. It is CRUCIAL for you to take your drops every day in order for them to have the proper effect in slowing down progression of the disease. We can’t stress enough how important it is to get into a routine for taking the drops. Countless people have lost their vision because they didn’t make a habit out of taking their drops. Just a few minutes a day can help you save your eyesight! If you have glaucoma, the most important thing for you to be aware of is that your level of cooperation in taking your glaucoma medications will determine how slow your vision deteriorates. The more consistently you take your drops = the better your vision will be. Make sure to schedule a visit to your eye doctor once a year to check for glaucoma!
Types of Glaucoma
Open angle glaucoma vs. angle closure glaucoma
- Open angle glaucoma
- In open angle glaucoma, optic nerve damage occurs even if your drainage structures appear “open”.
- Angle closure glaucoma
- In angle closure glaucoma, the drainage structures are “closed”, therefore raising the pressure inside your eye and damaging your optic nerve.
Both open angle and angle closure glaucoma can be broken down further into primary (unknown cause) and secondary (known cause) forms.
- Primary glaucoma refers to glaucoma that develops when there is high eye pressure without a specific cause.
- Secondary glaucoma refers to glaucoma in which there is a specific cause for higher than normal eye pressure, causing optic nerve damage and vision loss.
A Closer Look: Open angle glaucoma
Inside a normal eye, there is fluid, called aqueous humor, which is constantly being drained and renewed. This drainage system, similar to a drain in your sink that needs to stay clear to work properly, is meant to prevent any pressure build-up inside your eyes. In this form of glaucoma, the drainage structures of the eye are still “open”. So even though you might THINK that this allows you to still have normal eye pressure your eye pressure is STILL elevated!
So to sum up this type of glaucoma, if your drainage structures appear “open” and nothing else seems to be out of the ordinary but you still have some of the tell-tale signs of glaucoma, you have open-angle glaucoma.
But why does this pressure build-up happen although your drains are open? Here lies the difference between primary and secondary glaucoma. In primary open angle glaucoma: The short answer is – we don’t know! Long answer – there are various theories on why this is so, but at this point in time we can only assume that there are changes going on your eyes that are not able to be measured with the instruments available today. In secondary open angle glaucoma: There are many different causes of glaucoma:
- Angle recession: This refers to an injury to your eye causing damage to the “ciliary body” which is an important part of normal drainage of fluid in your eye.
- Uveitis: Swelling inside your eye can cause ‘garbage’ to block the anterior chamber angle, the fluid-filled space inside the eye between the iris and the cornea
- Pseudoexfoliation: This is a more general disorder in which abnormally high amounts of a protein-filled material is made in your eye. It is the most common cause of secondary glaucoma worldwide.
- Steroid response: Long-term use of steroids can cause high eye pressure leading to glaucoma.
Along with high eye pressure, all of these types of glaucoma will show specific types of defects on a side vision test, and will also causes changes on the optic nerve over time. The good news is that this is treatable with eye drops, laser or surgery as will be described in the treatment section.
Is it possible to have Glaucoma with a normal eye pressure?
YES! This is called, normal tension glaucoma. When primary open angle glaucoma occurs even with low eye pressure (usually said to be between 8 -20 mm/Hg) it is termed normal tension (or normotensive) glaucoma.
About ⅙ of patients in the United States with open angle glaucoma fall under the category of having normotensive glaucoma.
FYI: A recent school of thought is that these patients actually have thinner corneas (the front, clear surface of the eye) and therefore the pressure measurement is wrong. This means that even though the equipment used to measure reads a low number for the eye pressure, this number is actually much higher!
Angle-closure glaucoma
This form of glaucoma is characterized by the closing of the drainage structure called the anterior chamber angle. Since this is the part responsible for making sure the pressure in the eye does not rise, by draining the fluid made inside the eye, its closing causes higher eye pressure. This in turn causes glaucoma to develop.
Imagine holding a hose while water is turned on full-blast. You can picture how this can cause a severe increase in pressure!
Acute vs. Chronic forms of angle-closure glaucoma:
If you have acute angle-closure glaucoma, there is a sudden closing of the angle which leads to a tremendous increase in pressure in your eye, creating a sight-threatening emergency. In this case, your eye would be red and painful and you may experience headaches, nausea and blurred vision. If you are not treated in 24 hours, this condition may cause irreversible blindness.
In chronic angle closure glaucoma, part of your drainage angle closes occasionally and temporarily . This leads to a change from high to low pressure in your eyes but is not an emergency like the acute form.
Primary vs. Secondary:
Just as in open angle glaucoma, angle closure can also be broken down into primary or secondary forms.
- In primary angle closure glaucoma, the main reason for its development is unknown, but it results in the closing of most of the angle in your eye.
- In secondary angle closure glaucoma, there is an obvious cause, such as uveitis or neovascularization, or the growth of new blood vessels, into the angle itself.

Signs: How is glaucoma diagnosed?
1. Eye pressure
There is a strong connection between high eye pressure and the progression of glaucoma. However, your eye pressure does not have to be measured as high in order for glaucoma to develop.
FYI: It’s important to remember that just because you have high eye pressure; it does not mean you will develop glaucoma. Therefore, a high eye pressure alone is not enough for a doctor to diagnosis you with glaucoma. It can only be seen as a strong risk factor for developing glaucoma.
2. Visual field
Glaucoma generally affects your peripheral vision (side vision) first. In its early and even middle stages, glaucoma has no symptoms. Think about it: We often don’t even realize when things in our side vision are not quite as clear as they usually are since we’re usually paying closer attention to what’s straight ahead! Therefore, a test called a “visual field” is used to test your side vision.
3. Optical coherence tomography (OCT)
Optical coherence tomography (OCT) is a non-surgical, specialized camera that takes a detailed picture of the retina and the optic nerve. In this picture, your doctor can look at each individual layer of your retina as well as at all the cells that make up your optic nerve. This camera can detect any thinning of your optic nerve as well as identify differences in the thickness of the nerve as it changes over time.
This imaging is very helpful in detecting and monitoring glaucoma as well as many other retinal abnormalities, including macular edema.
4. Pachymetry
Your doctor may use pachymetry to measure your corneal thickness. There are several methods of performing pachymetry; some involve contact with your eye while others don’t touch the eye at all. The average corneal thickness is 555 microns (that’s 0.02 inches). Individuals with less than average thickness have a higher risk of developing glaucoma.
5. Gonioscopy
Gonioscopy is a procedure involving a hard contact lens which your doctor may utilize to carefully examine the drainage system of the eye. This special lens is used to magnify the small structures of the eye so that your eye doctor can detect any irregular qualities as well as determine whether there is anything clogging or closing your drainage system.
6. Fundus exam
A fundus exam is a close exam of the fundus (retina) with the use of magnification lenses. Your doctor will pay careful attention to the optic nerve, which is best seen through dilated pupils.
If you have glaucoma, the optic nerve appears “hollowed-out”. The nerve appears circular, like a donut, with a hole in the center which gets larger over time. As the glaucoma worsens, and optic nerve loses more and more nerve fibers, the hollowed out portion becomes larger. This is often called “cupping” by eye doctors. With glaucoma, the hollowed out portion of your optic nerve gets bigger over time which signifies more nerve damage.
Glaucoma Symptoms
- None!
- Fortunately or unfortunately, when glaucoma first develops, there are generally no symptoms. Symptoms only begin to appear at the very advanced stages of the disease.
- Tunnel vision:
- In advanced stages, you will have a significant loss of side vision and you may only be left with “tunnel vision” (see pic). If this happens, you may start bumping into walls and other things, not notice people at your sides, have an extremely difficult time driving and keeping up with your regular daily activities.
- Painful red eye
- In one type of glaucoma, called angle closure glaucoma, your eye becomes very red and painful, and you will experience blurry vision. This is an emergency and you will need to be taken to an emergency room or your eye doctor immediately.
- Nausea:
- With another type of glaucoma, called narrow angle glaucoma, you may experience nausea or dizziness when you go into a dark room. This happens when the drainage structures of your eyes have only a very narrow passage through which to drain fluid. In a dark room, your pupils dilate (or get bigger) and can cause your own iris (the colored part of your eye) to block the drainage angle. Similar to angle closure glaucoma, there is a quick increase in eye pressure that can cause you to feel nauseated or dizzy.
Glaucoma Risk Factors
African Americans
- Primary open angle glaucoma is six to eight -8 times more common in African Americans than in Caucasians.
Elderly
- Individuals over 60 years of age are six times more likely to get glaucoma.
Genetics
- Family history can increase the risk of glaucoma by four to nine times. This is especially true for siblings of glaucoma patients who have an even greater risk for developing Glaucoma.
Hispanics
- Hispanics over the age of 60 are at greater risk than those of European descent.
Asians
- In Asians, there is an increased risk of angle-closure glaucoma.
- Japanese are more at risk of developing normal tension glaucoma.
Steroid Usage
- Steroid use can increase the pressure in the eyes which can lead to glaucoma.
Inflammation
- Swelling inside the eye can cause debris to clog up the anterior chamber angle, raising eye pressure and leading to glaucoma.
Eye injury
- Even a minor injury to the eyes during sports can cause glaucoma later in life. With more than 1 million eye injuries occurring in the United States each year, it’s important to know that after an eye injury has happened, an eye exam with an ophthalmologist is important to monitor the eye for any developing glaucoma.
Pseudoexfoliation
- Pseudoexfoliation is an aging–related disease primarily affecting the eyes, in which there is a buildup of microscopic protein fibers. If you have this condition, you have a y, significantly increased risk of developing glaucoma.
High myopia
- Due to areas of thinning around the optic nerve, if you are very nearsighted, your optic nerve is more prone to damage and may develop glaucoma. Other research shows that extremely nearsighted eyes have specific features that can increase their risk of glaucoma.
Is There a Cure for Glaucoma?
Unfortunately, there is no known cure for glaucoma at this time. Moreover, most factors that put you at risk for developing glaucoma, such as age and race, are not preventable. At this time the only factor your doctor may be able to control is eye pressure.
Glaucoma Treatments: How To Control Eye Pressure
Laser: Sometimes drops just don’t cut it
- When drops are not providing enough treatment or you are having a difficult time remembering to put in the drops, your doctor may recommend laser treatment.
- Laser treatments are a very common procedure in which a laser is applied to the iris (colored part of the eye) in order to create additional pathways for the eye fluid to drain.This in turn will help lower your eye pressure.
- Two commonly performed laser treatments:
- Laser peripheral iridotomy (LPI)
- This may be performed if you have very narrow angles, in order to create another path for fluid to drain out of your eye.
- Selective Laser Trabeculoplasty (SLT):
- A laser procedure that creates small burns in one of your drainage structures, called the trabecular meshwork. This gives you a larger area through which the eye fluid can drain.
- Argon Laser Trabeculoplasty (ALT):
- An older alternative to SLT but not performed quite as often.
- Laser peripheral iridotomy (LPI)
- Two commonly performed laser treatments:
1. Drops
With dosing anywhere from one to four times per day per eye, this is by far the most common way to treat glaucoma.
- There are a few different categories of eye drops which can help lower your eye pressure. One type can decrease the amount of fluid made in your eye and another improves the drainage system of the eye so that the fluid can drain more easily.
- Often, your doctor will prescribe more than one medication if you have an advanced case of glaucoma.
- The current medications used are:
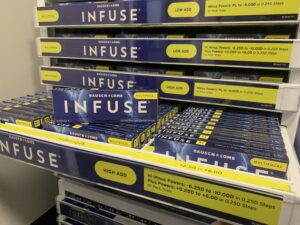
- Prostaglandin analogs
- The current medications used are:
- Often, your doctor will prescribe more than one medication if you have an advanced case of glaucoma.
- Alpha agonists
- Carbonic anhydrase inhibitors
2. LASER
- When drops are not providing enough treatment or you are having a difficult time remembering to put in the drops, your doctor may recommend laser treatment.
- Laser treatments are a very common procedure in which a laser is applied to the iris (colored part of the eye) in order to create additional pathways for the eye fluid to drain.This in turn will help lower your eye pressure.
- Two commonly performed laser treatments:
- Laser peripheral iridotomy (LPI)
- This may be performed if you have very narrow angles, in order to create another path for fluid to drain out of your eye.
- Selective Laser Trabeculoplasty (SLT):
- A laser procedure that creates small burns in one of your drainage structures, called the trabecular meshwork. This gives you a larger area through which the eye fluid can drain.
- Argon Laser Trabeculoplasty (ALT):
- An older alternative to SLT but not performed quite as often.
- Laser peripheral iridotomy (LPI)
- Two commonly performed laser treatments:
3. Surgery
Trabeculectomy:
- During a trabeculectomy a triangular cut is made in your sclera (the white part of the eye), a drainage hole is created and a “bleb” pooling of aqueous from the new hole is formed. This leads to more efficient draining which will in turn lower your eye pressure.
Surgical implant/shunt:
- The reason your doctor may consider placing a surgical implant with a shunt or tube in your eye is to more aggressively attempt to lower your eye pressure by creating a new path for the fluid to drain.
Since there are many forms of shunt surgeries performed, they are not all outlined here. Ask your doctor for more information if you will be having this type of surgery.