Keratoconus Specialists in Michigan
Scleral Lenses May Be For You
What is Keratoconus?
Keratoconus is a progressive eye disease in which the normally round, dome-shaped cornea becomes thin and cone-shaped. This abnormal shape causes light rays to focus incorrectly on the retina, resulting in distorted or blurred vision. Keratoconus can occur in one or both eyes and is usually diagnosed in people in their teens or early 20s. The condition typically progresses slowly and may stabilize after several years.
Symptoms of keratoconus include distorted or blurry vision, sensitivity to light, glare, and halos around lights. In advanced stages of the disease, the cornea may bulge out so much that it becomes difficult to wear contact lenses or to see clearly even with glasses.
There is no cure for keratoconus, but treatments are available to manage the condition and improve vision. These treatments may include eyeglasses, special contact lenses, or surgery. It is important for people with keratoconus to see an eye care professional regularly to monitor the progression of the disease and to receive appropriate treatment.
Treatment for Keratoconus
Treatment options may include eyeglasses, special contact lenses, corneal cross-linking, or corneal transplant surgery, depending on the severity of the condition and the specific needs of the patient. Regular monitoring by an eye care professional is important to manage the condition and improve vision.
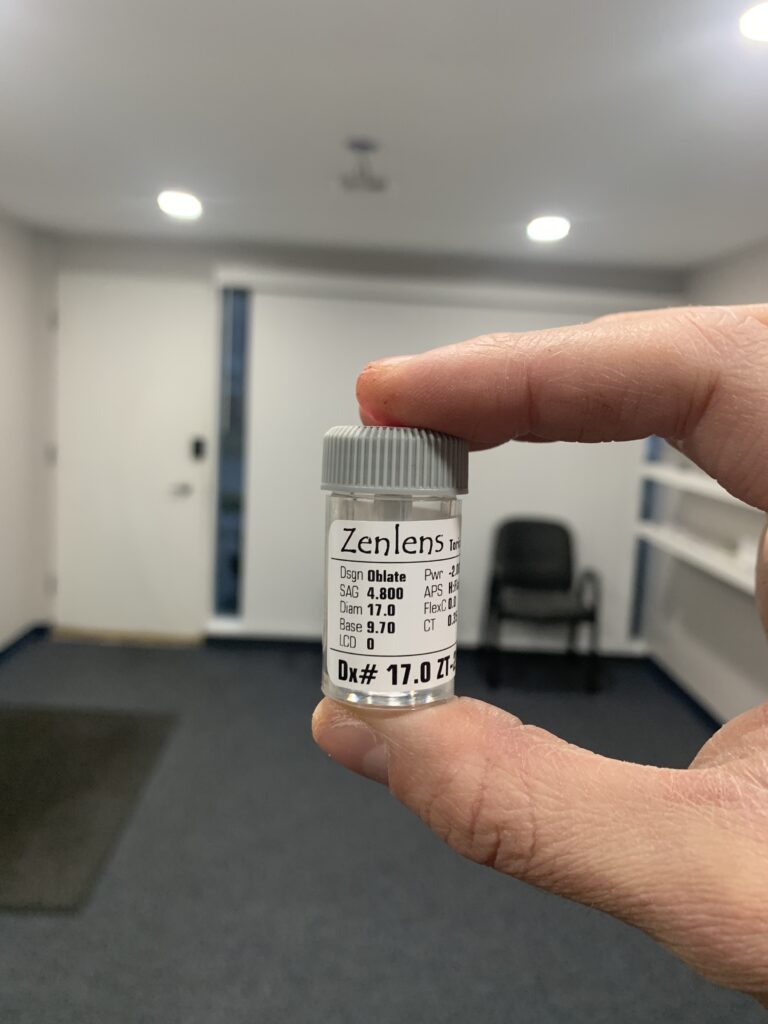
Scleral Lenses
At Michigan Contact Lens, our Optometrists frequently recommend scleral lenses as a solution for individuals with keratoconus. These lenses are designed to fit over the cornea, rather than directly on it, which makes them more comfortable for people with this condition.
Scleral lenses are filled with a non-preserved sterile saline solution, which helps to keep the lens lubricated and helps to compensate for surface irregularities on the cornea. This can provide the comfort of a soft lens with the optical quality of a gas-permeable lens.
Additionally, scleral lenses are designed to stay stable on the eye with little or no movement during blinks, which is an advantage over traditional corneal gas permeable lenses. Overall, scleral contact lenses are considered the best option for providing health benefits and increased comfort compared to smaller corneal rigid lenses or soft lenses.
Corneal Collagen Crosslinking treatment for Keratoconus and Post-Lasik Ectasia
A common treatment for keratoconus and post-Lasik ectasia is called Corneal Collagen Crosslinking (CXL). This treatment is designed to strengthen the cornea by increasing the crosslinking, or bonding, of the collagen fibers within the cornea. This helps to stabilize the cornea and prevent further thinning and distortion, which can improve visual acuity in most patients.
The CXL treatment process involves applying a solution of riboflavin (a vitamin) to the surface of the cornea, followed by exposure to ultraviolet A (UVA) light. The combination of the riboflavin and UVA light helps to increase the crosslinking of the collagen fibers in the cornea.
CXL treatment is typically performed on an outpatient basis and takes about an hour. Most patients experience a temporary decrease in vision after the treatment, but this usually improves within a few days. While CXL treatment has been shown to be effective in slowing the progression of keratoconus and improving visual acuity in most patients, it is not a cure for the condition and some patients may still need to use glasses or contact lenses after the treatment. Our team at Michigan Contact Lens is here to help you determine if CXL treatment is the right option for your specific needs.

AvaGen Genetic Testing for Keratoconus
This test is designed to help identify genetic markers that may increase a person’s risk of developing keratoconus or predict the likelihood of the progression of the condition.
The AvaGen test involves a simple saliva sample, which is then analyzed in a laboratory to identify specific genetic markers associated with keratoconus. At Michigan Contact Lens, we offer AvaGen Genetic Testing to help identify genetic markers that may increase a person’s risk of developing keratoconus or predict the likelihood of progression of the condition. When you undergo AvaGen testing with us, your sample is collected and sent to a laboratory for analysis. The lab then returns a comprehensive report that provides a full risk assessment for keratoconus, as it is the most common corneal disorder.
In addition to evaluating the risk for keratoconus, the report also examines any variant forms of the condition to provide more precise treatment options. It also includes a full risk assessment for other corneal dystrophies, based on specific genes that are known to be the leading cause of these conditions.
The report includes a deep interpretation of the variant data and what it means for you as the patient. This information can be used to guide treatment decisions and monitor the progression of the condition, helping to preserve the health and function of your eyes.
Our team at Michigan Contact Lens will work with you to determine if AvaGen Genetic Testing is the right option for you. Understanding the potential genetic factors that may be contributing to your keratoconus can help us tailor a treatment plan to best meet your specific needs and help to preserve the health and function of your eyes.