Michigan's Contact Lens Specialists
Looking for a Keratoconus Doctor in Michigan?
It's time to meet with the best!

Finding The Best Keratoconus Doctor Near You
Receiving a diagnosis of Keratoconus can be unsettling. This progressive eye condition, which causes the cornea to thin and bulge into a cone shape, can lead to significant vision distortion that glasses can’t always fix. The journey ahead can feel uncertain, and the most important first step is finding the right expert to guide your care.
Your search for a top keratoconus doctor in Michigan ends here. At Michigan Contact Lens, our clinic is a center of excellence for the diagnosis and management of keratoconus. We understand the unique challenges this condition presents and are dedicated to using the most advanced technology and treatments to protect and restore your vision.
This comprehensive guide will walk you through everything you need to know about keratoconus, from early symptoms and diagnosis to the full spectrum of modern treatment options. We’ll show you why choosing a true specialist is critical and how our team provides the expert care you need.
What is Keratoconus?
Keratoconus is a progressive eye condition that affects the cornea, the clear, dome-shaped surface of the eye. In a healthy eye, the cornea has a round shape, but in keratoconus, the cornea thins and begins to bulge outward into a cone shape. This structural change prevents light from focusing correctly on the retina, leading to significant visual challenges.
This condition typically begins in the teenage years or early 20s and can worsen over time if not managed properly by a qualified keratoconus doctor in Michigan. According to the National Keratoconus Foundation, it affects approximately 1 in every 2,000 individuals. Left untreated, keratoconus can severely impact vision and quality of life, making tasks like driving at night or reading difficult and frustrating.
Causes and Risk Factors for Keratoconus
The exact cause of keratoconus is not fully understood, but it is believed to be linked to a combination of genetic, environmental, and biochemical factors. A keratoconus specialist in Michigan will consider all these factors during your evaluation.
Genetic Predisposition
Genetics play a significant role. About 1 in 10 people with keratoconus have a parent who also has the condition. It is also more common in individuals with certain systemic conditions like Down syndrome, Ehlers-Danlos syndrome, and other connective tissue disorders.
Chronic Eye Rubbing
There is a very strong association between chronic, vigorous eye rubbing and the progression of keratoconus. The physical stress and friction from rubbing can weaken the already compromised corneal structure. This is often linked to conditions that cause itchy eyes, such as allergies, atopic dermatitis, or eczema.
Collagen Abnormalities & Oxidative Stress
The cornea is primarily made of interwoven collagen fibers that give it strength and shape. In keratoconus, these fibers are weaker. It is believed that an imbalance in enzymes within the cornea leads to oxidative damage, which further weakens the collagen and allows the cornea to bulge.
A Closer Look at the Symptoms of Keratoconus
The symptoms of keratoconus can be subtle at first but typically worsen as the cornea becomes more irregular. It’s crucial to see a doctor if you experience any of the common signs of keratoconus.
Blurry and Distorted Vision
This is the primary symptom. It’s not the same as normal nearsightedness. Patients often describe it as looking through a warped or wavy window. Straight lines may appear bent or crooked.
Increased Sensitivity to Light (Photophobia) and Glare
The irregular cone shape of the cornea scatters light as it enters the eye instead of focusing it cleanly. This causes disabling glare from sources like headlights, streetlights, and even computer screens, making night driving particularly difficult.
Frequent Prescription Changes
One of the earliest red flags for a developing keratoconus is a rapid and frequent change in an eyeglass prescription, especially a significant increase in astigmatism. If your vision seems to be getting noticeably worse every year, it warrants a specialist evaluation.
Monocular Diplopia (“Ghost Images”)
This is a hallmark symptom of keratoconus. It’s the perception of a faint, transparent second image trailing the primary one, like a comet’s tail. If you cover one eye and still see double or multiple images, it’s a clear sign of a corneal irregularity.
Eye Strain and Headaches
The brain works incredibly hard to try and make sense of the poor-quality, distorted images it’s receiving from the affected eye. This extra effort can lead to persistent eye strain and headaches.
How a Keratoconus Diagnosis in Michigan is Made
A definitive diagnosis is the first and most important step. A comprehensive eye exam by our keratoconus doctor in Michigan will include several painless, advanced tests:
- Corneal Topography: This is the gold standard for a keratoconus diagnosis in Michigan. It’s a non-invasive imaging test that creates a detailed, 3D color map of the cornea’s surface. This map instantly reveals any cone-like steepening or irregularities that are invisible to the naked eye.
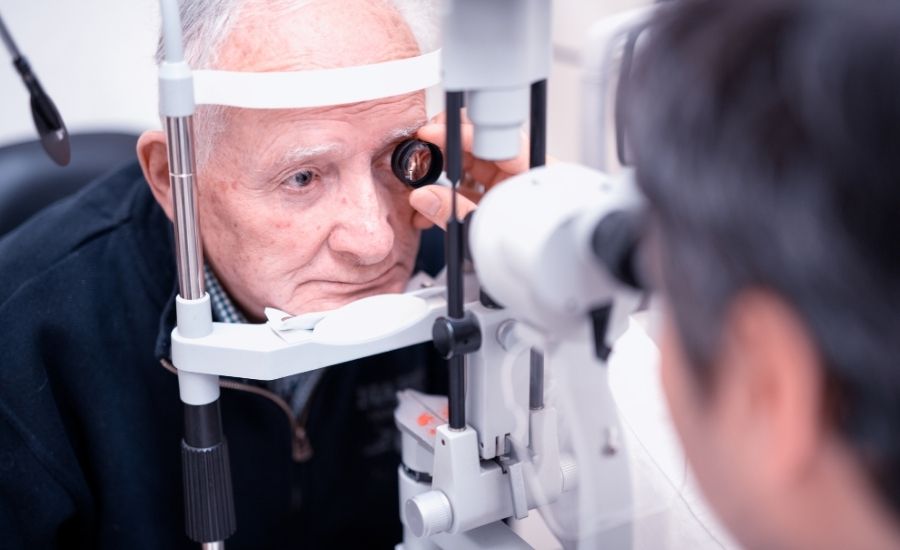
- Slit-Lamp Examination: A high-magnification microscope is used to observe for clinical signs of keratoconus, such as corneal thinning, Fleischer rings (iron deposits at the base of the cone), or Vogt’s striae (fine stress lines in the cornea).
- Pachymetry: This test uses ultrasound to precisely measure the thickness of the cornea. Significant thinning, especially in specific areas, is a key indicator of keratoconus.
Early detection is crucial for effective management, allowing for interventions that can halt the progression of the disease.
A Full Spectrum of Keratoconus Treatment in Michigan
The right keratoconus treatment in Michigan depends on the stage and progression of the condition. Our goal is always twofold: first, stop the condition from getting worse, and second, provide the best possible vision.
1. Corneal Cross-Linking (CXL): Halting Progression
Corneal Cross-Linking (CXL) is a revolutionary, minimally invasive procedure and the only treatment proven to stop keratoconus from getting worse. It is a vital early intervention to preserve the cornea’s integrity.
The procedure involves applying riboflavin (Vitamin B2) eye drops to the cornea, which are then activated by a controlled UV light. This process creates strong new bonds between the collagen fibers in the cornea, making it stronger and more stable. As noted by the American Academy of Ophthalmology, CXL is highly effective at preventing the need for future, more invasive surgery. We work with the top surgeons for corneal cross linking in Michigan to co-manage your care.
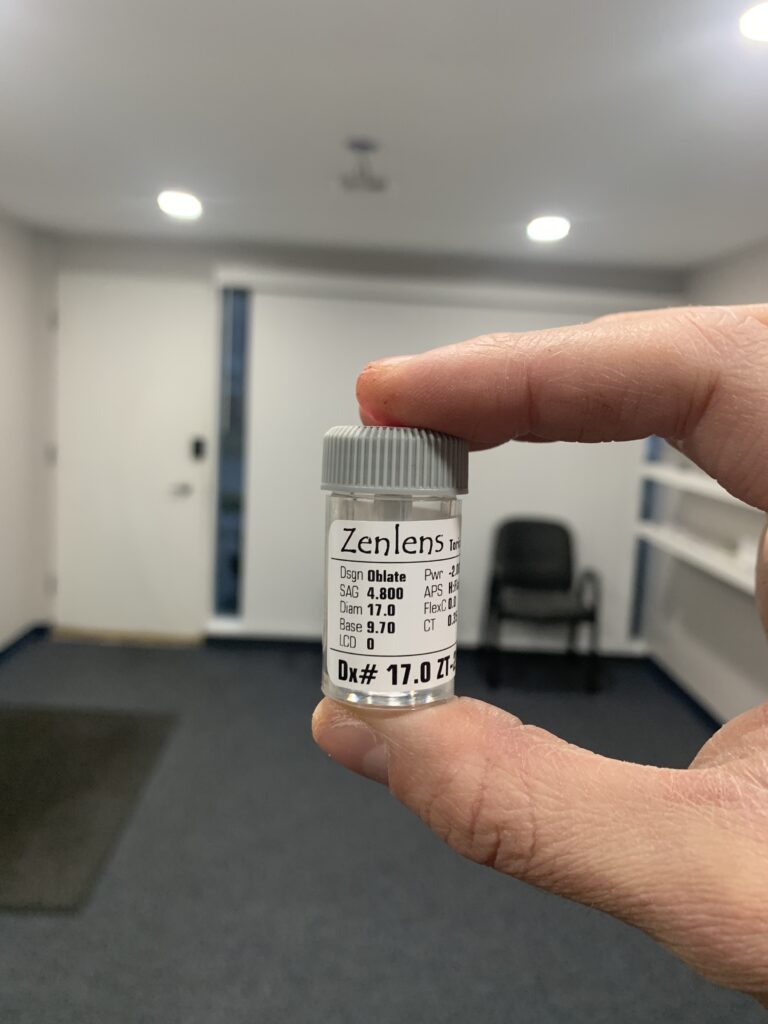
2. Scleral Lenses: The Premier Non-Surgical Vision Solution
For restoring clear vision, the premier non-surgical keratoconus treatment is a custom-designed scleral lens. These large-diameter lenses vault completely over the irregular cornea, creating a perfectly smooth optical surface. The space between the lens and the eye is filled with saline, neutralizing all distortions.
The fitting process for these lenses is complex and requires advanced technology and expertise. However, the result is often life-changing, providing a level of comfort and clarity that no other non-surgical option can match. Our clinic is a leading provider of scleral lenses for keratoconus in Michigan.
3. Other Custom Contact Lenses (RGP & Hybrid)
In some mild or moderate cases, smaller Rigid Gas Permeable (RGP) lenses or hybrid lenses (with a hard center and soft skirt) can also be effective at improving vision. Our specialists will determine the best option for your specific corneal shape.
4. Surgical Options (for Advanced Cases)
For the most advanced cases where the cornea is significantly scarred or contact lenses are no longer effective, surgical intervention may be required. This can include a partial-thickness transplant (DALK) or a full-thickness corneal transplant (PKP). Our keratoconus doctor in Michigan will co-manage your care with the best corneal surgeons in the state.
Scleral Lenses Solution by Keratoconus Doctor in Michigan
At Michigan Contact Lens, our keratoconus doctor in Michigan will often recommend scleral lenses as the premier vision-correcting option for individuals with moderate to advanced keratoconus. These lenses rest on the stable, less sensitive sclera (the white of the eye), completely vaulting over the irregular cornea.
The space between the lens and the cornea is filled with sterile saline, which creates a perfectly smooth new optical surface and enhances comfort by constantly bathing the eye in moisture. The custom fit of scleral lenses for keratoconus in Michigan provides the clarity of gas-permeable lenses with the comfort of soft lenses, ensuring stability and minimal movement during blinks.
This makes them a superior option for managing keratoconus compared to traditional lenses, and fitting them correctly is a hallmark of the best keratoconus doctor in Michigan.
Your Keratoconus Questions Answered
Is keratoconus treatment covered by medical insurance?
In most cases, yes. Keratoconus is a medical diagnosis, not a routine vision issue. As such, medically necessary treatments, including procedures like Corneal Cross-Linking and specialty contact lenses like sclerals, are often covered by medical insurance plans, not just vision plans. Our team can help you navigate your benefits.
Can I get LASIK if I have keratoconus?
No. LASIK is strictly contraindicated for patients with keratoconus. The procedure involves thinning the cornea, which would dangerously weaken an already compromised keratoconic eye. A thorough screening by a keratoconus specialist in Michigan is essential to rule out the condition before any refractive surgery.
How often do I need to see my keratoconus doctor?
Follow-up schedules vary depending on the severity and stability of your condition. Patients with progressive keratoconus may be seen every 3-6 months to monitor for changes, while those with stable vision in well-fitting scleral lenses are typically seen annually by their keratoconus doctor in Michigan.
Please call our keratoconus doctor near you for more Keratoconus information.
Schedule Your Consultation with a Leading Keratoconus Doctor in Michigan
Don’t let the uncertainty of a keratoconus diagnosis control your life. With modern treatments and expert care, clear, comfortable vision is achievable. The first step is a consultation with a true specialist.
Contact Michigan Contact Lens today to schedule your comprehensive evaluation. Let our team show you the path to better vision.

